
An advance directive is a document that allows a person (“principal“) to select someone else (“agent“) to make medical decisions on their behalf. The directive also allows a person to make a declaration detailing the health care preferences if they can’t speak for themselves (e.g. reject artificial feeding and breathing machines). An advance directive must be signed in accordance with State law for it to be legal for use.
Signing Requirements (State-by-State laws) – In most cases, an advance directive must be signed by a notary public or two (2) witnesses.
Getting an advance directive does not cost any money and can be done on a do-it-yourself basis. The truth is most attorneys use the same templates provided by the State . It’s always recommended to seek legal advice but this can be done yourself and 100% free.

An Advance directive is usually split up into 4 parts (depends on the State):
All parts of an advance directive are recommended to be completed to give medical staff the best idea of your medical treatment preferences for any situation.

The Principal will need to decide their medical treatment options. It’s best to review the Advance Directive and discuss medical treatment options with family. Once decided, it’s time to complete the living will portion of the form and decide to also have a Health Care Agent.
If a Health Care Agent is selected, they will generally follow the recommendations made by the Principal in the living will portion of the document. The Agent, commonly a spouse or family member, will be the one that ultimately makes the decision to reject or accept life-sustaining treatment (i.e. ventilators, artificial nutrition, etc.)
Even though it is highly recommended to have a Health Care Agent, it is not required.

In some States, as an additional option, the Principal may be able to make decisions about their immediate treatment (DNR) or organ donation (anatomical gift).
Download and complete the form in its entirety. After completing, be sure to sign in accordance with State law. If a notary public is required, you can choose to find a local notary or use an online service like Notarize.com ($25).

Although it is not required, it’s best to store the document with a county , state , or commercial registry. Otherwise, handing the copies off to the agent and close family members is the next best thing.
In the event of an emergency, make sure a wallet card is always on the Principal sharing where the advance directive is located. This will be the first place paramedics will check to find any healthcare treatment preferences.
Includes forms, signing requirements (with laws), and main laws
| State | Signing Requirements | Statutes |
| Alabama | Two (2) witnesses | § 22-8A-4(4) |
| Alaska | Notary public or two (2) witnesses | § 13.52.010 |
| Arizona | One (1) witness or a notary public | § 36-3221, § 36-3224, § 36-3262 |
| Arkansas | Two (2) witnesses or a notary public | § 20-6-103, § 20-17-202 |
| California | Two (2) witnesses or a notary public | PROB § 4673(3), PROB § 4701 |
| Colorado | Two (2) witnesses or a notary public | § 15-18-106 |
| Connecticut | Two (2) witnesses | Sec. 19a-575, Sec. 19a-575a |
| Delaware | Two (2) witnesses | § 2503(b) |
| Florida | Two (2) witnesses | § 765.202(1), § 765.302(1) |
| Georgia | Two (2) witnesses | § 31-32-5(c)(1) |
| Hawaii | Two (2) witnesses or a notary public | §327E-3 |
| Idaho | Principal only | § 39-4510 |
| Illinois | Two (2) witnesses | 755 ILCS 35/3(b), 755 ILCS 45/4-10 |
| Indiana | Two (2) witnesses | § 16-36-1-7, § 16-36-4-8, § 16-36-4-11, |
| Iowa | Two (2) witnesses and a notary public | § 144B.3(b) |
| Kansas | Two (2) witnesses and a notary public | § 58-632, § 65-28,103 |
| Kentucky | Two (2) witnesses or a notary public | § 311.625(2) |
| Louisiana | Two (2) witnesses | RS 28:224, RS 40:1151.4 |
| Maine | Two (2) witnesses | §5-803.2 |
| Maryland | Two (2) witnesses | § 5-602(c) |
| Massachusetts | Two (2) witnesses | § 201D-2 |
| Michigan | Two (2) witnesses | § 700.5506(4) |
| Minnesota | Two (2) witnesses | § 145C.03 |
| Mississippi | Two (2) witnesses | § 41-41-205(2.a), § 41-41-209 |
| Missouri | Two (2) witnesses and a notary public | § 459.015, § 404.705 |
| Montana | Two (2) witnesses and a notary public | § 50-9-103, § 53-21-1304(2)(d) |
| Nebraska | Two (2) witnesses or a notary public | § 30-3404, § 20-404 |
| Nevada | Two (2) witnesses | NRS 162A.790 , NRS 449A.433 – 39 |
| New Hampshire | Two (2) witnesses | § 137-J:14 |
| New Jersey | Two (2) witnesses | NJ Rev Stat § 26:2H-56 |
| New Mexico | Principal only | NM Stat § 24-7A-2 |
| New York | Two (2) witnesses | PBH § 2981 |
| North Carolina | Two (2) witnesses and a notary public | § 32A-16(3), § 90-321(3) |
| North Dakota | Two (2) witnesses or a notary public | § 23-06.5-05(2) |
| Ohio | Two (2) witnesses or a notary public | § 2133.02(A)(1), § 1337.12(A)(2) |
| Oklahoma | Two (2) witnesses | § 63-3101.4(A) |
| Oregon | Two (2) witnesses or a notary public | § 127.515, § 127.527 |
| Pennsylvania | Two (2) witnesses | § 5442, § 5452 |
| Rhode Island | Two (2) witnesses or a notary public | § 23-4.11-3(a), § 23-4.10-2 |
| South Carolina | Two (2) witnesses | § 62-5-503, § 62-5-504, § 44-77-40 |
| South Dakota | Two (2) witnesses or a notary public | § 59-7-2.1, § 34-12D-2 |
| Tennessee | Two (2) witnesses or a notary public | § 34-6-203, § 68-11-1803(b) |
| Texas | Two (2) witnesses or a notary public | § 166.003, § 166.154, § 166.164 |
| Utah | One (1) witness | § 75-2a-107(c) |
| Vermont | Two (2) witnesses | § 9703 |
| Virginia | Two (2) witnesses | § 54.1-2983 |
| Washington | Two (2) witnesses or a notary public | § 11.125.050, § 70.122.030 |
| Washington D.C. | Two (2) witnesses | § 7-622, § 21-2205 |
| West Virginia | Two (2) witnesses and a notary public | § 16-30-4 |
| Wisconsin | Two (2) witnesses | § 155.10, § 154.03(1) |
| Wyoming | Two (2) witnesses or a notary public | § 35-22-403(b) |
Depends on the situation and jurisdiction. If a medical power of attorney was authorized, the agent will have the ultimate decision-making power. If the agent happens to be a family member, then they may be able to override the treatment options in the living will.
It is required to be notarized in the states of Iowa, Kansas, Missouri, Montana, North Carolina, and West Virginia. In all other states, an advance directive can be signed with two (2) witnesses only.
Depends on the laws in the State. Individuals that commonly cannot act as witnesses are:
List all health care treatment options in the chance you cannot speak for yourself. This also includes in the event you become incapacitated with no chance for a cure, to proceed with or without life-sustaining procedures.
An Agent is recommended to have someone in case representation is needed (cannot speak for yourself). Depending on the State, there may be optional items such as organ donation (“anatomical gift”).
Some States have official registries while others do not have a place to file an advance directive. There are commercial websites a person can use that will hold their document like ___ ($_/yr) and ___ ($__/yr).
Every holder of an advance directive should carry a wallet card. A wallet is usually the first place medical personnel looks when identifying a patient.
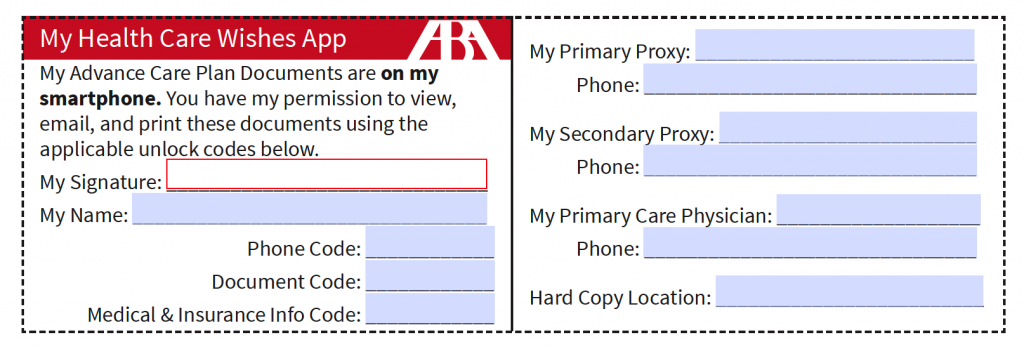
America BAR Assoc Wallet Card
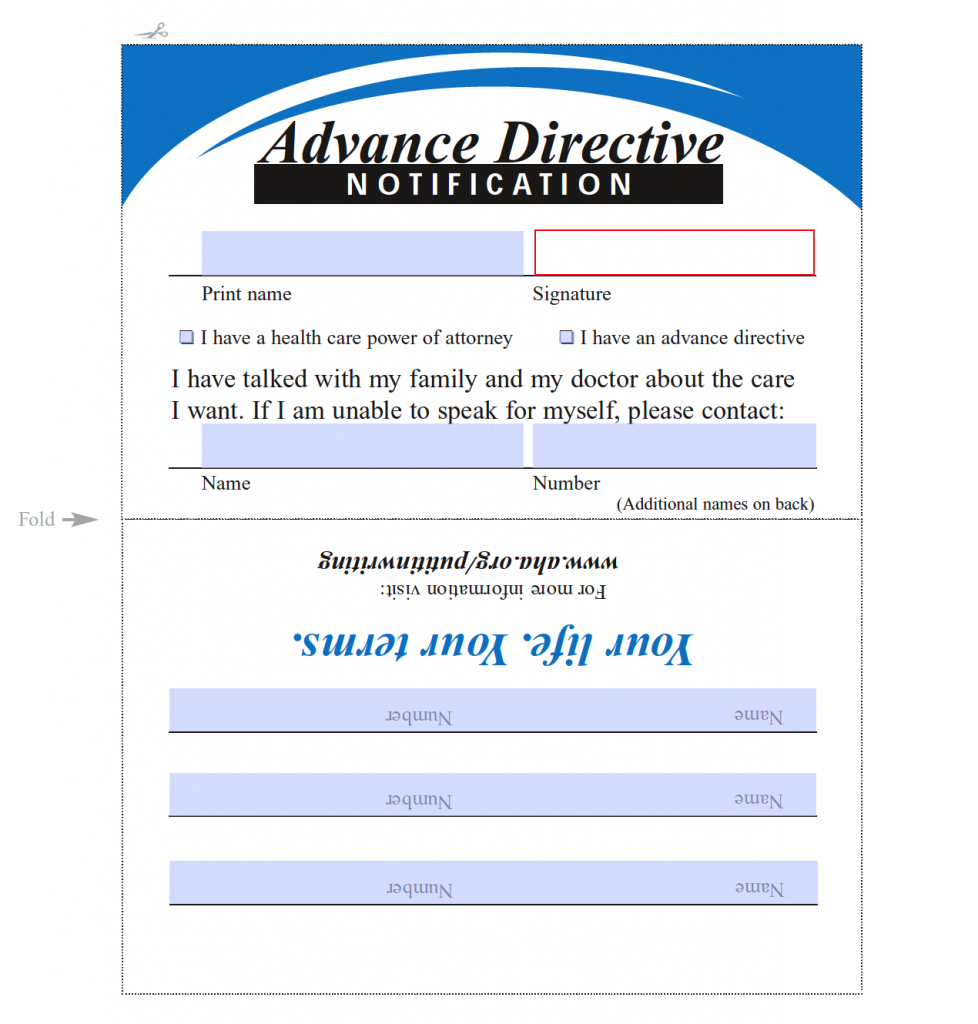
American Hospital Assoc. Wallet Card
Advance Directive – Or “Health Care Directive” is a document that combines a medical power of attorney, living will, and other estate documents to plan one’s end of life treatment options.
Anatomical Gift – Otherwise known as organ donation.
Agent – Or “Health Care Agent”, “Proxy”, or “Attorney-in-Fact” is someone that is able to speak on your behalf in the chance the Principal is not able to do so.
Do Not Resuscitate (DNR) – Or “MOST”, “POST”, or “POLST” is a form that outlines a patient’s medical treatment options. Common for patients with terminal conditions to detail whether or not they would like to receive life-sustaining procedures.
Living Will – Or “Directive” that informs medical staff of their intentions in the chance they can no longer speak for themselves. Commonly will outline their preference to reject artificial breathing and nutrition.
Notary Public – A that is licensed in a specific State to handle acknowledging legal documents such as Advance Directives.
Medical Power of Attorney – Or “Health Care Proxy” or “Durable Health Care Form” which allows a person to select someone else to make health care decisions on their behalf.
Principal – The person the advance directive is for and the Agent will represent.
Witness – A witness is an individual over the age of 18 years (19 in some States) and viewed the Principal authorizes an Advance Directive. In some States, there are restrictions on who may act as a witness.
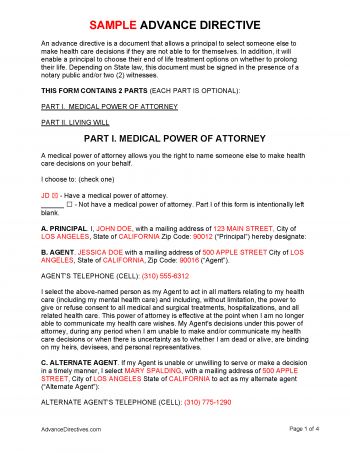
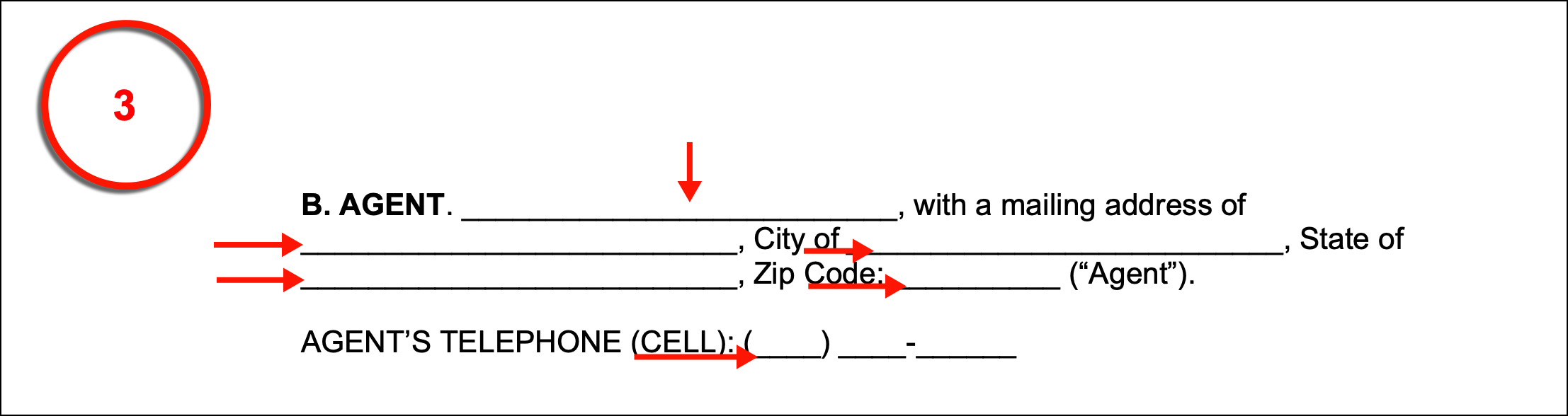
(1) Power Of Attorney Status. The template package will allow you to include a Medical Power Of Attorney. If a medical condition or trauma has rendered you unable to communicate with attending Medical Staff, then an authorized Medical Attorney-in-Fact can be approached to issue your consent or refusal to medical treatment. This requires a significant amount of faith in your Attorney-in-Fact, thus, you may elect to include such an appointment from this packet or you may exclude it. In either case, this decision must be reflected by marking one of the two checkboxes then delivering your initials to the left.
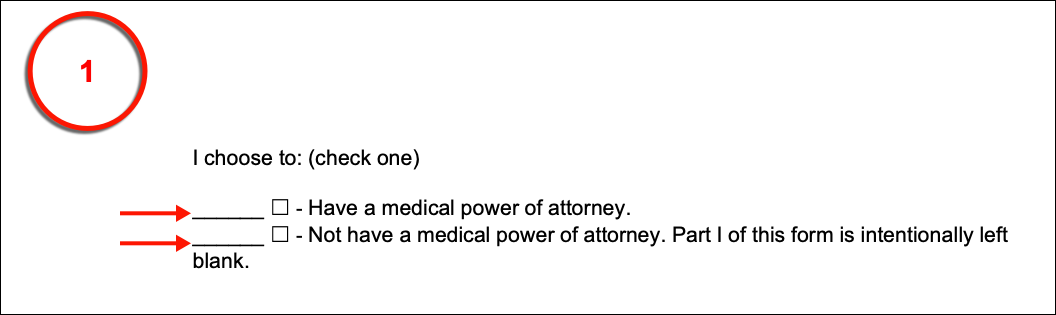
(2) A. Principal. As mentioned earlier, when you fill out this document, you will assume the role of the Principal who shall appoint a Medical Attorney-in-Fact or Health Care Agent to speak to Doctors with the goal of deciding upon your medical treatment. This Agent can have as much or as little power as you like. To proceed, list your full name, address, city, state, and zip code.
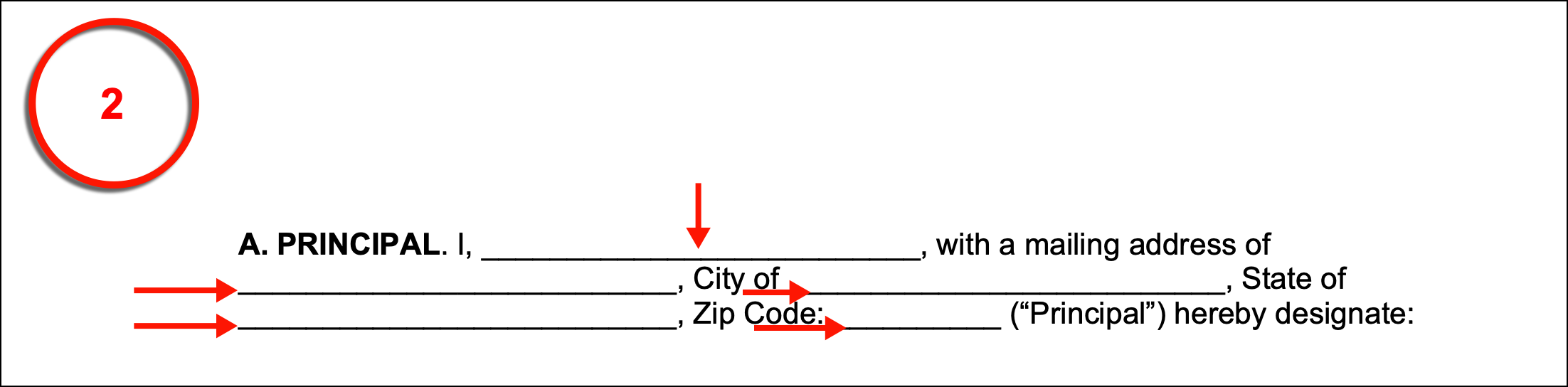
(3) B. Agent. The Medical Attorney-in-Fact is often commonly referred to as your Health Care Agent or simply your Agent. This will be the Private Party that shall be kept informed on your medical preferences and have a clear idea of what your decisions in various medical scenarios would be. Assign this Party to the Medical Attorney-in-Fact role by dispensing his or her full name, mailing address, city, state, zip code then his or her current cell phone number. Bear in mind, that Physicians or Responders reviewing this document in your medical records may need to contact this Agent immediately, thus, make sure this is an up-to-date and reliably maintained phone number of the Agent.
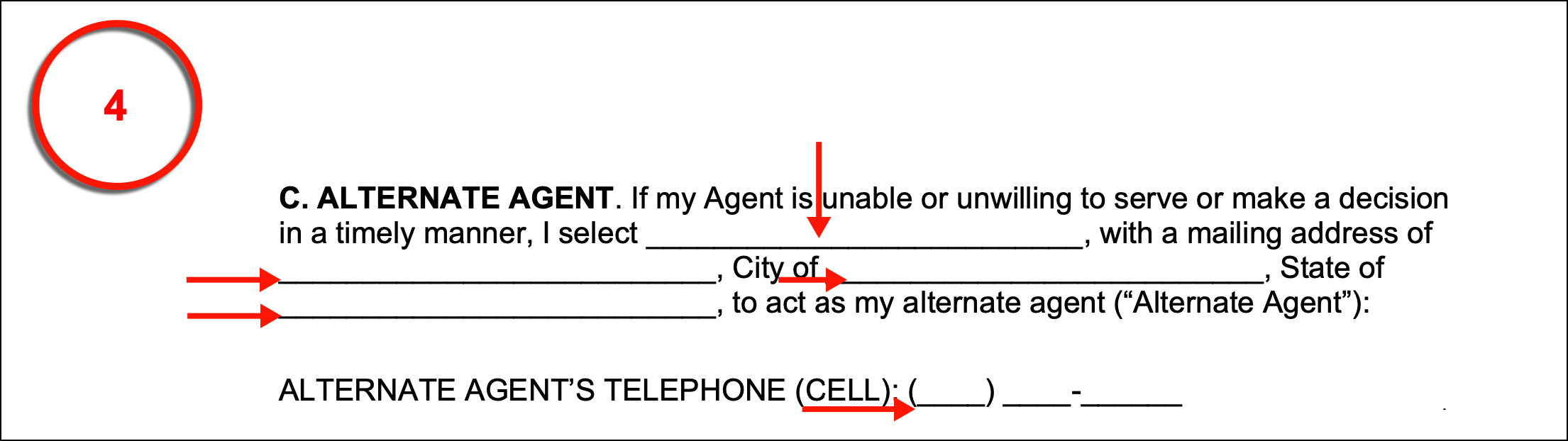
(4) C. Alternate Agent. The Private Party named as Attorney-in-Fact may fail in this role either by choice or by circumstance. For instance, he or she may become incapacitated, have to travel for an extended period of time, or become disqualified (i.e. a revocation or unwilling to act). If this should happen while you are incapacitated, then you could be left without a Medical Attorney-in-Fact at a time when you rely on him or her heavily. This situation may be dealt with in this form by establishing an Alternate Agent who has already been approved for the Medical Attorney-in-Fact role. To take advantage of this option, he or she must be identified by name, mailing address, city, state, zip code as well as his or her cell phone number.
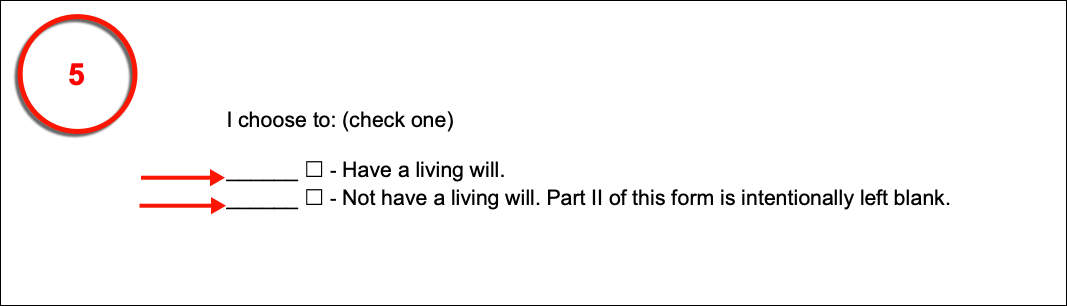
(5) Living Will Status. The second portion of this package allows you to declare specific wishes regarding medical treatment when you are experiencing an end-of-life medical event. This document also needs an indication regarding whether it shall be included or not. Demonstrate this status by selecting the appropriate checkbox statement then initialing it.
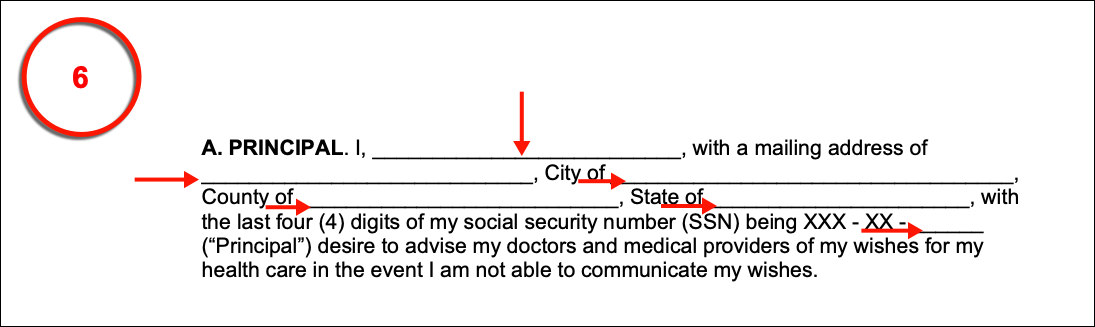
(6) A. Principal. If you have decided to include the living will, then you must claim the role of its Principal. This requires your full name, mailing address, city, county, state, and the last four digits of your social security number.
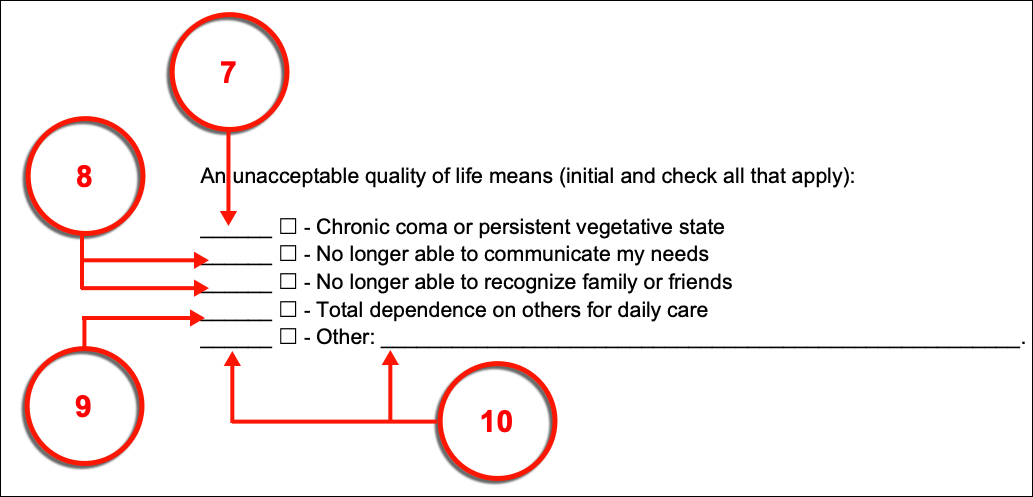
(7) B. Life Support. Your directions regarding the treatment goals attending Physicians should adopt when you are uncommunicative and experiencing an end-of-life condition will need to be defined clearly. The language informing Medical Personnel that you wish life support withdrawn should your Physicians formally declare that no treatment will result in an unacceptable recovery has already been provided however, your definition of an unacceptable recovery is needed. A list of quality of life issues will enable you to what you consider an unacceptable quality of life by checking the corresponding checkbox then, providing your initials. For instance, by selecting the first checkbox statement and initialing your approval you will inform Physicians that you consider being in a coma or being in a persistent vegetative (i.e. unconscious) is unacceptable to you and that you will not consent to life-support treatment should this be a permanent state of life after recovery.
(8) Social Inability. The second and third statements respectively declare that recovering but losing the ability to communicate your needs and/or recognize your loved ones (i.e. family, friends, etc.) would be unacceptable. You may select one or both of these statements by marking the appropriate checkbox and providing your initials as needed.
(9) Dependence. The fourth predetermined statement allows you to inform Physicians that being completely dependent on others for your day-to-day needs (i.e. brushing your teeth, bathing, etc.) would be an unacceptable definition for recovery if you select it and dispense your initials.
(10) Principal Definitions. A final option that allows you to define recovery scenarios that you would be unable to live with is available. This requires your direct input and you must select then initial the corresponding checkbox area to show of your approval.
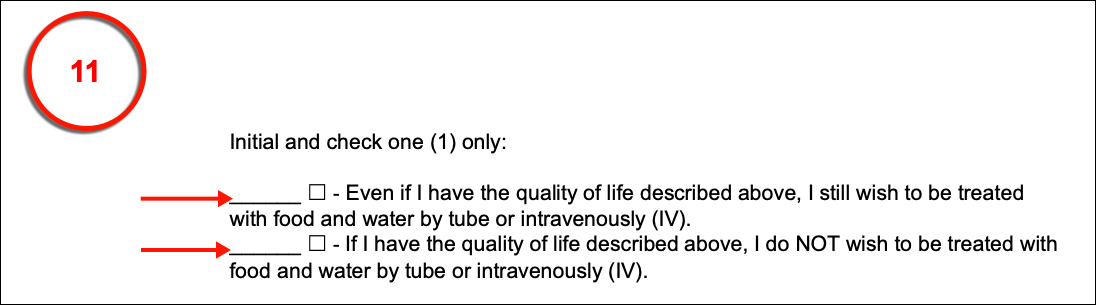
(11) Intravenously Administered Food And Fluids. An important consideration to make will be whether you consent to food and water being administered with a tube or intravenously when you are suffering an end-of-life event. You can inform Physicians that you wish to receive food and water under any circumstances or that you intend to refuse artificially administered food and water if your current (or future) quality of life is unacceptable.
(12) C. Certain Life-Sustaining Treatment. Cardiopulmonary Resuscitation (CPR). It is now time to address the treatments that are commonly applied in response to a life-threatening medical event. Cardiopulmonary Resuscitation, (known as CPR) is used when the heart and/or lungs can no longer perform well enough to maintain consciousness and/or life. To inform Medical Responders that you will not consent to the administration of care when you experience a cardiopulmonary failure, you must select the first checkbox then display your initials.
(13) Ventilation (Breathing Machine). If you are unable to breathe independently, attending Health Care Staff will attempt to extend your life by artificially delivering oxygen to your lungs (often) through a tube connected to your air pipe or lungs. To deny this treatment, select the third checkbox then deliver your initials as verification.
(14) Feeding Tube. Physicians may direct Medical Staff to deliver food and fluids in an attempt to maintain your nutrition levels at an acceptable level for survival. You can refuse to consent to this procedure through this paperwork by marking the checkbox corresponding to the fourth statement of this section and initialing the left-hand margin.
(15) Dialysis. Vital organs such as your kidneys may cease functioning. In a case where your kidneys fail, you will be unable to survive for any extended period of time thus, attending Medical Personnel (such as Physicians or Nurses) will seek your consent to maintain your kidney functions with a dialysis machine. This document will enable you to communicate to such Personnel that you will not consent to be maintained on a dialysis machine by selecting and initialing the fourth item.
(16) Principal Directive. You can issue concerns, refusals, or conditions of consent to other treatments for medical scenarios not discussed thus far by entering your directives in the space corresponding to the final statement choice. If needed, you can deliver such instructions or provisions on an attachment that is named in this choice. Be advised that you must still mark the checkbox on display and deliver your initials.

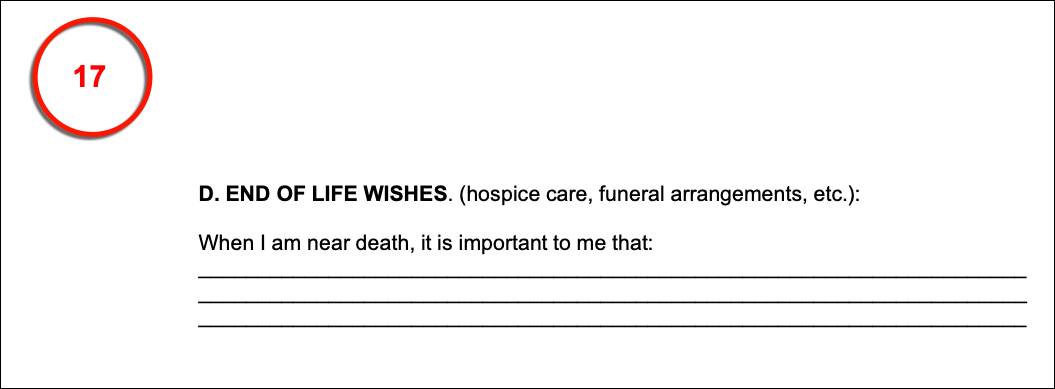
(17) D. End Of Life Wishes. You can directly address your loved ones and other concerned Parties with your preferences, wishes, or expectations with additional end-of-life concerns such as funeral arrangements, religious or spiritual needs, and hospice care in the final area. This can be produced directly in the document being worked on or placed in a titled attachment that is cited properly by name.
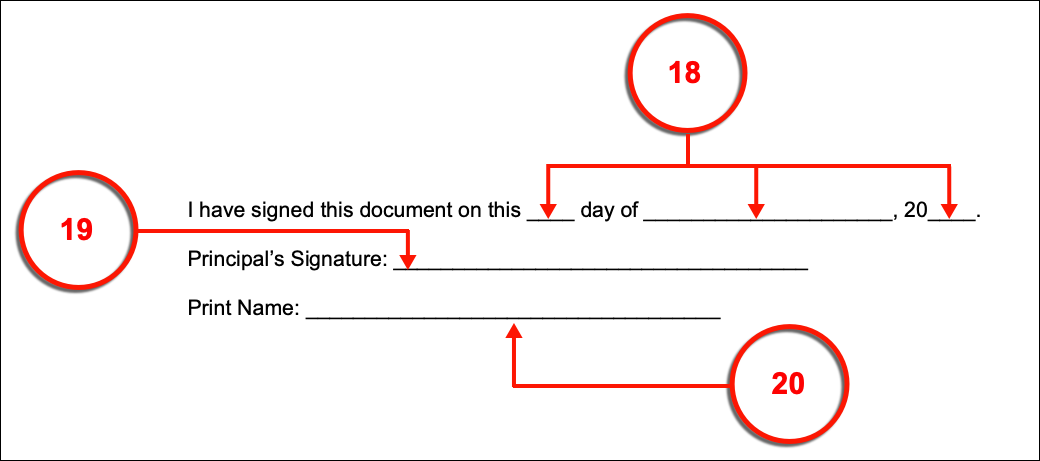
(18) Signature Date. Document the calendar date immediately before proceeding to sign this paperwork.
(19) Principal Signing. Make sure you are familiar with your State’s guidelines for executing this document. Oftentimes, your signature will need to be witnessed, notarized, or both. When you have gathered the appropriate Parties for this signing, produce your signature.
(20) Principal Name. Print your name
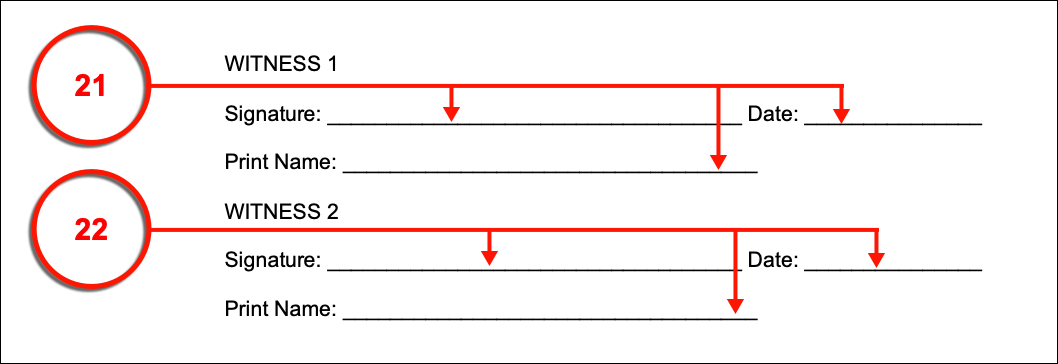
(21) Witness 1. The first Witness must read the declaration beneath your signature. Witness 1 must show agreement with this statement by producing his or her signature, the current date, and his or her printed name. Once done, Witness 1 should relinquish this document to the next Party (as needed).
(22) Witness 2. If a second Witness is required then he or she must also attest to the testimonial by signing his or her name, reporting the current calendar date, then delivering his or her printed name.
(23) Notary Public. If your act of signing must be notarized, then make sure that a Notary Public recognized by the State where your directives will be effective is on-hand during your execution of this paperwork. The Notary Public is the only Party that can subject your signature to the notarization process as proof of its authenticity.